Managing The Supermarket With Type 2 Diabetes
Supermarkets can often be difficult to manage when you’re following a healthy eating plan. With special offers on each shelf and an overwhelming amount of tempting products, where even the ones claiming to be “healthy” are most likely not, it can be challenging to know where to start.
For those with type 2 diabetes, prediabetes, or other symptoms of metabolic syndrome, where a healthy lifestyle can help manage it, it’s important to know exactly what you’re looking for before you leave for the shops. A list in hand is the best way to keep on track and with these helpful tricks, you’ll be in and out in no time.
To learn more about diabetes, you can read about it here.
What foods to include
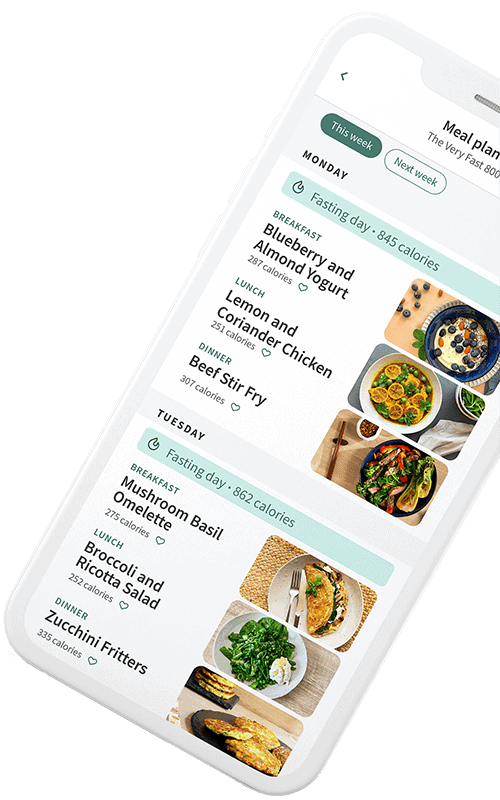
Plan out your meals for the week ahead, write down your ingredients and break down the macros ensuring you’re achieving enough protein, fibre and healthy fats in your diet to keep you full on a calorie deficit low enough to help you lose weight. This really is key to your success; great meal planning means you’re more likely to stick to your healthy plan and less likely to find your way to aisles packed with processed foods. If you’re struggling to find the time to do your meal planning, our Programme can do it for you with structured meal plans developed and calculated by our nutrition team. Learn more about it here.
Fresh vegetables and fruit
Low calorie, non-starchy vegetables should be eaten liberally. Include a variety of colours to ensure you consume a range of nutrients and make the most of their disease-fighting benefits.
Although starchy vegetables and fruit can be added to your diet, we recommend that you enjoy them every now and then; starchy vegetables and fruit are higher in carbohydrates, meaning they will have an impact on your blood sugars. To manage blood sugar spikes, when you’re eating starchy vegetables and fruit, enjoy them as part of a meal high in protein and healthy fats to slow the release of insulin and manage hunger levels.
Lean meat and oily fish
Oily fish is a fantastic source of omega-3 fatty acids, recommended for good heart health. Studies have recognised that oily fish may be linked to a reduced risk of type 2 diabetes.[1] With multiple health benefits, many leading authorities recommend eating a fish based meal at least twice a week, with one of these servings being an oily fish such as salmon, mackerel or sardines. Further to this, oily fish is a good source of vitamin D; research recognises that vitamin D levels are often lower in those with type 2 diabetes, or at risk of type 2 diabetes.[2]
Opt for lean meats; lean meats are a good source of protein, an important macronutrient for those at risk of type 2 diabetes, or those that might already have the condition. Protein keeps you fuller for longer, curbing your appetite for snacks throughout the day. Snacking spikes your insulin levels between meals and tends to increase hunger. Try to avoid snacks, especially on fasting days, but if required, have some non-starchy vegetables, a sliver of cheese or some berries. Alternatively, nuts are a great source of protein, fibre and micronutrients – just avoid salted or sweetened nuts, which can be moreish and easy to overeat.
Full fat dairy
While full fat dairy may be slightly higher in calories than low fat varieties, it’s far more filling and satisfying, lower in sugars and free from artificial flavours and sweeteners.
To assess the impact of dairy, The PURE Study (2020)[3] took 113,000 participants from 21 countries, all between the ages of 35-70, and assessed their dietary intake over an average course of nine years. The results were remarkable – those who consumed two portions of full-fat dairy each day had a 28 per cent lower risk of developing metabolic syndrome when compared to those who adhered to a dairy-free diet. Additionally, those who consumed dairy had a lower risk of developing type 2 diabetes and high blood pressure.
When you’re spoilt for choice at the supermarket, always opt for Greek yogurt over low fat, or flavoured options. Greek yogurt is higher in protein and lower in carbohydrates, which will overall stabilise any blood sugar spikes.
Join our email community
Learn more about The Fast 800 approach to healthy living by receiving our free content, health tips and recipes as well as exclusive offers, delivered straight to your inbox.
Extra virgin olive oil
Along with oily fish, we encourage adding extra virgin olive oil to meals. A splash makes vegetables taste better and improves the absorption of fat-soluble vitamins. For cooking, use olive or coconut oil. Avocado is another great source of healthy fats that will keep you feeling full and satiated.
There is also evidence to show that the body’s glycaemic response (the effect that food or meal has on blood glucose levels after consumption) can be reduced with the addition of olive oil to a meal.[4] In a small study that compared olive oil to corn oil, participants that consumed olive oil with each meal experienced smaller spikes in their blood sugar levels, when placed against those adding corn oil.[5]
In addition to this extra virgin olive oil contains anti-inflammatory compounds, such as oleic acid, omega-3 fatty acids and polyphenols. This reduction in inflammation in the body can have positive effects on depression and gut health.
“It’s always a good idea to read ingredient labels and check for quality certification as there are plenty of olive oils on the market that do not have the same quality as a cold-pressed extra virgin olive oil”
– Gabi, The Fast 800 Nutritionist
Legumes
A low carb Mediterranean-style diet does not mean no carbs at all. Not only is this very difficult to achieve, but can be detrimental. This is why complex carbs and fibre are still important and can easily be gained from vegetables, legumes and wholegrains.
Fibre can be separated into two types: soluble and insoluble fibre, both of which have their own benefits. Soluble fibre dissolves in water whereas insoluble fibre doesn’t, yet both have great benefits. Soluble fibre aids digestion and helps to reduce blood sugar levels, which can assist in reducing the risk of insulin resistance and type 2 diabetes. Insoluble fibre also helps to reduce the risk of type 2 diabetes and promotes bowel regularity by adding water to stools, preventing constipation.
Legumes to add to your trolley:
- Kidney Beans
- Cannellini Beans
- Lentils
- Edamame beans (often found in the frozen section)
- Chickpeas
Wholegrains include:
- Brown rice quinoa
- Bulhar (cracked wheat)
- Whole rye
- Whole grain barley
- Wild Rice
- Buckwheat
The Fast 800 Programme can help with editable meal plans that generate shopping lists so you know exactly what to get for the week to make each healthy, Mediterranean-style meal. If you’re cooking for family and friends, you can edit your serving sizes and the shopping list will automatically update, taking away any calculations.
If you’ve been thinking about it for a while, but are still a little unsure if it’s right for you, you can try it first for free, for 7 days.
Money saving tips
- Frozen vegetables are a great option for soups and curries.
- Try shopping online to avoid getting tempted by the special offers on each aisle.
- Check the labels and seek out the ingredients, you may be able to make your own version. Rather than buying pre-prepped porridge or muesli, often packed with added sugars and calories, you can easily make your own – here’s our simple recipe.
- Fermented foods can often be expensive and sometimes have hidden sugars. If you wish to purchase at the supermarket, just be sure to check the ingredients. Alternatively, it’s quite simple to make your own and incredibly cost effective, you just need a little patience. Here’s an easy recipe to get you started.
- Tinned foods are also a great option, and just as nutritious. Be sure to check the ingredients and make sure there are no hidden nasties.
Chen GC, Arthur R, Qin LQ, Chen LH, Mei Z, Zheng Y, Li Y, Wang T, Rohan TE, Qi Q. Association of Oily and Non Oily Fish Consumption and Fish Oil Supplements With Incident Type 2 Diabetes: A Large Population-Based Prospective Study. Diabetes Care. 2021 Mar;44(3):672-680. doi: 10.2337/dc20-2328. Epub 2021 Jan 11. PMID: 33431419; PMCID: PMC7896269.
Kayaniyil S, Vieth R, Retnakaran R, Knight JA, Qi Y, Gerstein HC, Perkins BA, Harris SB, Zinman B, Hanley AJ. Association of vitamin D with insulin resistance and beta-cell dysfunction in subjects at risk for type 2 diabetes. Diabetes Care. 2010 Jun;33(6):1379-81. doi: 10.2337/dc09-2321. Epub 2010 Mar 9. Erratum in: Diabetes Care. 2011 Jan;34(1):247. PMID: 20215450; PMCID: PMC2875459.
Bhavadharini B, Dehghan M, Mente A, et al Association of dairy consumption with metabolic syndrome, hypertension and diabetes in 147 812 individuals from 21 countriesBMJ Open Diabetes Research and Care 2020;8:e000826. doi:10.1136/bmjdrc-2019-000826
Bozzetto L, Alderisio A, Giorgini M, Barone F, Giacco A, Riccardi G, Rivellese AA, Annuzzi G. Extra-Virgin Olive Oil Reduces Glycemic Response to a High-Glycemic Index Meal in Patients With Type 1 Diabetes: A Randomized Controlled Trial. Diabetes Care. 2016 Apr;39(4):518-24. doi: 10.2337/dc15-2189. Epub 2016 Feb 9. PMID: 26861923.
Violi F, Loffredo L, Pignatelli P, Angelico F, Bartimoccia S, Nocella C, Cangemi R, Petruccioli A, Monticolo R, Pastori D, Carnevale R. Extra virgin olive oil use is associated with improved post-prandial blood glucose and LDL cholesterol in healthy subjects. Nutr Diabetes. 2015 Jul 20;5(7):e172. doi: 10.1038/nutd.2015.23. PMID: 26192450; PMCID: PMC4521177.